All we need to know about selective laser trabeculoplasty
All we need to know about selective laser trabeculoplasty
What is selective laser trabeculoplasty (SLT), and what is it used to treat?
It is considered effective as a primary treatment for open-angle glaucoma, including pigmentary glaucoma, and in patients with ocular hypertension. SLT can be used as adjunct therapy in patients currently using glaucoma medications, and it is effective when medications have failed. SLT is not recommended for neovascular glaucoma.
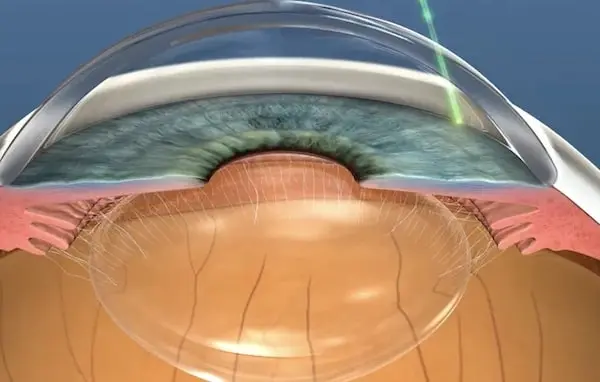
SLT is described as « selective » because the laser targets only specific cells in the trabecular meshwork.Selective laser trabeculoplasty (SLT) is a relatively new development in glaucoma therapy. SLT is a safe, widely effective, and virtually painless approach to lowering intraocular pressure. As with other types of laser trabeculoplasty, the goal of SLT is to open the drainage angle to allow the eye’s natural fluid to drain out, thus reducing intraocular pressure. What sets SLT apart as a treatment alternative is that it does not produce the cellular damage to the trabecular meshwork associated with other forms of laser treatment; this, in turn, means that SLT can be safely repeated in the future.
What does SLT consist of? Is it painful?
SLT is a simple outpatient procedure, which can be performed by your ophthalmologist in the clinic. Before the procedure begins, patients may be asked to discontinue certain glaucoma medications. Eye drops to lower intraocular pressure generally are continued. The pupil may be constricted with special eye drops called miotics to prevent a temporary increase in intraocular pressure after the procedure. One or more types of anaesthetic are used to numb the eye and the surrounding area.
In the first step of the procedure, the ophthalmologist examines the meshwork drainage area of the eye through a special lens. Then, a beam of light is applied to the drainage area for a very short period of time. This is not to be felt or cause damage to the outer part of the eye, but instead affects the pigment. The pigment will then be washed away naturally by the body’s immune system over the next few days or weeks. This will allow the drainage area to function more effectively, gradually lowering the IOP.
Typically, slt is not a painful procedure. There is no discomfort of the eye during or after the procedure. This, it differs greatly from alt which uses a higher energy beam that can cause scarring to the eye and some discomfort. Slt can be quite accurately described as a quick stinging sensation which is over within a second. This may be felt several times, depending on the number of spots that are required to complete the procedure.
How successful is selective laser trabeculoplasty? Can I undergo it more than once?
Repeatability of SLT
SLT can be repeated successfully when the effect is declining and has been shown in some studies to achieve a similar effect compared to the initial treatment. As it is a noninvasive treatment with no thermal effects or structural changes in the tissue, repeat treatments are unlikely to cause any abnormal or unwanted effects. The safety of re-treatment has been demonstrated in both animal studies and clinical trials. In one clinical study, repeat SLT treatments resulted in an increase in the IOP lowering effect along with a prolonged period of maintaining the result achieved after the first and second treatments. In another study, some patients who did not respond to the initial treatment showed a good long-term effect with subsequent treatments.
Probable success of Selective Laser Trabeculoplasty
There is a large body of evidence to back the use of SLT. The recent Glaucoma Laser Trial supports the evidence that SLT is at least as useful as argon laser trabeculoplasty. Other smaller investigations have shown good success rates of 63-70% at 6 months. The effect of SLT in the long-term appears to be much better than that of argon laser trabeculoplasty. Studies have shown that the intraocular pressure lowering effect of ALT tends to fade after the first year of treatment. On the other hand, SLT has shown consistent good results at various time points over the course of 3 years.
Is it a safe procedure?
Generally speaking, selective laser trabeculoplasty is a safe procedure, but like any procedure it carries risks. The laser has been in existence for over three decades and the existing background information supports the thought that SLT is safe. However, take into account that no surgical procedure is totally risk free. The most commonly reported complication following SLT is a transient IOP (intraocular pressure) spike. This can occur in approximately 15% of treated patients and usually resolves spontaneously within 24 hours. There are rare reports of post-operative inflammation, cystoid macular edema (CMO) and peripheral anterior synechiae following SLT treatment. These side effects are usually managed effectively with steroid treatment and are self-limiting, with minimal or no long-term effect on vision or corneal endothelial cell count. SLT is safe in that it is repeatable and has no risk of causing structural or cellular damage to the trabecular meshwork, thus leaving pressure levels in untreated areas of the meshwork unaltered. This is particularly important in having a safe alternative to medication in the treatment of normal tension glaucoma where lowering IOP without causing hypotony is the key to preventing progression.
Are there any related side effects? If so, what are they?
Slt has been shown to be very safe at decreasing IOP with minimal side effects. Usually, the most common side effect, occurring in 20% of treatments, is a transient IOP spike of >5mmHg in the immediate postoperative period which resolves within 24 hours of the procedure and can be managed with short-term use of topical antiglaucoma medications. The main concern with SLT is the potential risk for inflammation in the anterior chamber « uveitis ». Rates vary from 0-6.5% and are managed using topical steroids for roughly a week following the procedure. Though very rare cases may need oral steroids for up to 4 weeks. Although no cases of long-term corneal endothelial cell loss or visually significant cataract formation associated with SLT have been reported, patients with Fuch’s Dystrophy or cell count of less than 2000 should be informed that there is a potential risk for corneal decompensation from an inflammatory response in the endothelium.
Routine prophylactic anti-inflammatory treatment has not been shown to affect efficacy outcomes and SLT may be performed safely in patients with concomitant glaucoma and dry age-related macular degeneration with no significant change in visual function at 1 year post-treatment. Overall, the treatment has significantly less risk compared with ALT, particularly in the incidence of IOP spikes within the first 24 hours post-treatment, the risk of long-term IOP elevation, and subsequently the need for more aggressive medications to control IOP.

