Cornea Transplant Surgery: What You Need to Know
Cornea Transplant Surgery: What You Need to Know
Who Needs One?
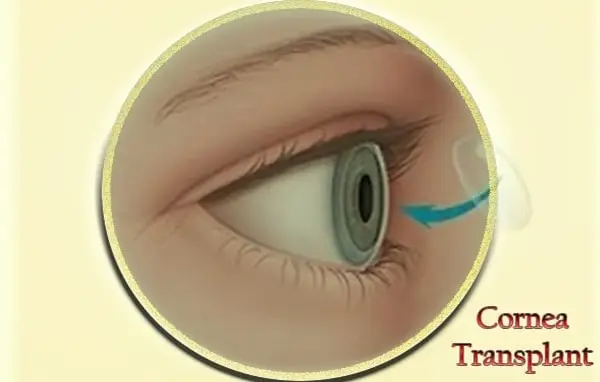
Not everyone with corneal damage needs a corneal transplant. It’s usually considered when other treatments don’t work. A corneal transplant can be a good way to restore clear vision because it replaces the damaged tissue on the eye with healthy corneal tissue from a donor. The common reasons for needing a corneal transplant include having eye conditions which affect the cornea such as: Fuchs’ dystrophy, where the inner layer of the cornea fails; keratoconus, a condition which causes the cornea to become cone-shaped and change. Scars, due to injury or infection such as an eye infection with the herpes simplex virus (herpes keratitis). I have keratoconus and had a transplant on my left eye a few years ago. Keratoconus is the most common reason to have a corneal transplant in the UK. Honestly, the thought of having a transplant and what the procedure involved made me feel a bit nervous, but knowing that corneal transplant surgery has a good success rate and can restore clear vision really helped me to feel better about it. Also, knowing that this type of operation has been performed for over 100 years and among the most common and successful transplant operations made me feel confident that everything would be okay. Some conditions, such as keratoconus, may only need a part of the cornea to be replaced and this can be done with a more modern procedure called deep anterior lamellar keratoplasty (DALK). This type of transplant doesn’t replace all the layers of the cornea, but it involves taking away the part that’s damaged. I had the more traditional type of corneal transplant called penetrating keratoplasty, which replaces all layers of the cornea. However, there have been huge advances in corneal transplant techniques and procedures and there are lots of different methods available; you should discuss the most suitable option with an eye specialist. Rapid changes in technology are also leading to new possibilities to help people needing corneal transplants. For example, researchers are investigating ways to grow corneal tissue in the laboratory so that donor corneas may not be needed in the future.
Full Thickness Corneal Transplant
Many ophthalmic surgeons prefer the term « keratoplasty » to corneal transplant surgery. The term keratoplasty refers to surgery that is performed on the cornea and is used generically, without specifying the method of obtaining or the type of the corneal transplant material. This type of surgery may be used if the cornea is damaged due to an injury that affects all layers of the cornea. It may also be used if a person’s cornea is not of a naturally clear shape or is not uniformly curved, for example if a person has had the condition keratoconus. A full thickness corneal transplant is a complex operation which involves removing all of the naturally occurring layers of the cornea, called a « host cornea », and replacing it with these same layers from a donor cornea. The donor cornea is placed into the eye and the layers are held in position by using one very tiny nylon stitch that is removed approximately one year after surgery. The stitches are so fine that, in everyday light, you can’t see them. We use a transilluminator which is a special light that shines through the stitches to help us see the sutures when we remove them. After the operation there is a chance that the new cornea will be rejected by the person’s own immune system. To help prevent this, patients will need to take steroid eye drops for many months after the surgery. The drops will be used very frequently at the start and then the dose will be decreased over time. Because the stitches do not dissolve, there will always be a small risk that the new cornea will be rejected from years after surgery but it is perfectly possible for a full thickness corneal transplant to last for many years.
Partial Thickness Corneal Transplant
When discussing corneal transplantation techniques, I would like to go over the various procedures that fall under the category of partial thickness transplants or endothelial keratoplasty. The first procedure we will discuss is the Descemet’s Stripping Endothelial Keratoplasty or DSEK. This procedure was developed as a less invasive alternative to the traditional full thickness corneal transplant. DSEK has been found to have faster recovery times and better visual outcomes compared to the full thickness transplant. This is because the major incisions in the full thickness procedure are replaced by smaller incisions in the DSEK procedure. This results in less trauma to the eye structures and subsequently less chance of complications from surgery as well as better refractive outcomes in the short term. The basic method of performing DSEK involves removing the patient’s endothelial layer and replacing it with donor endothelium and stroma. The first step in DSEK is ensuring that the patient’s cornea is the correct thickness for the procedure to be successful. Using specialized ultrasound mapping of the cornea – known as Pachymetry, the surgeon will measure the thickness at various points with the centre having a target thickness of between 500 and 600 micrometres. This is important as a cornea that is too thin can result in the surgeon inadvertently breaching the posterior corneal stroma and causing a full thickness perforation. Likewise, a cornea that is too thick can make it very challenging to successfully replace the abnormal endothelium and avoid complications from surgery.
Endothelial Keratoplasty
Instead of replacing the entire cornea, as in traditional keratoplasty, only the thin layer of cells lining the inside of the cornea is replaced in endothelial keratoplasty. This layer of cells is called the endothelium, and in the three types of endothelial keratoplasty (Descemet’s stripping endothelial keratoplasty or « DSEK », Descemet’s membrane endothelial keratoplasty or « DMEK », and Descemet’s membrane endothelial keratoplasty with « pre-stripped tissue »), different parts of this layer are replaced. DSEK replaces the endothelium plus a thin layer of stroma (the main part of the cornea). DMEK replaces only the endothelium. In all three procedures, the host (the patient receiving the transplant) endothelium and some stroma are removed and the donor tissue is put into place. The host tissue then regenerates over the donor tissue. These procedures require a thinner, partial thickness corneal donor graft, rather than a full thickness graft used in traditional transplant. This means that the surgery is less invasive and risky, and the recovery time is usually shorter. However, partial thickness corneal grafts also require more technical skill to place and secure, and the success of the transplant is more dependent on the skill and preference of the surgeon; for DSEK and DMEK, success rates can be up to 70%.
What’s the Surgery Like?
Well, for one thing, the surgery won’t happen until a matched donor becomes available. For more information on this, you might find it helpful to read our series Starting Points to Transplantation. Secondly, from start to finish, the actual surgical time lasts from 3 to 12 hours. It starts with a nurse or orderly collecting you from the hospital ward that you’re staying in and taking you down to the preoperative ward of the operating theatre. There, the nurses check you in and ask you a lot of questions about your health. You might have noticed that I’ve emphasized matched donor in the paragraph above. It’s really important that the new corneas should have as many things in common with your own corneas as possible. So the surgical team are looking for a donor who has the same approximate corneal width and curvatures as your own. After all the preparations have been done, including the cold packs being applied and the local anesthetic eye drops being used, testing for feeling and light in the eye, not to mention marking which eye is going to be operated on, the surgeons are then ready to remove the old opaque cornea. The steps of an eye operation involve the microscope focusing on the cornea. Next, once the old cornea has been removed, whether by being cut or ‘peeled’ off, the new cornea is carefully sewn into place. Finally, the plastic shield or small dressing is placed over the newly operated eye. The whole operation is called a corneal transplant or keratoplasty, from the Greek roots ‘kerato’ meaning cornea and ‘plasty’ meaning formative process / operation. The type of keratoplasty that you have depends upon what layer of the cornea is being replaced. My donor cornea was only used to replace the top layer or ‘skin’ of the cornea, formally known as the ‘epithelium’. This is called LK, or Lamellar Keratoplasty, and as a result of this kind of surgery, the eye’s healing time is much reduced.
Recovery
The recovery period from eye transplant surgery is usually swift, although some discomfort and continued enhancement to setting may be experienced for a number of weeks or even months. Patients are generally permitted to go home within a number of hours of the transplant surgery, although somebody else will have to drive and it might be necessary to put on protective shields over the eyes thoroughly, particularly when sleeping. Patients themselves are advised to take things very easy for at least a week after returning home, although most can get back to work and restart driving after approximately a fortnight. It is important to prevent rubbing or touching the eyes at all costs for some time after surgery, as any damage could lead to the transplant becoming dislodged as a result. The eyes are rather sensitive to light and heating throughout the recovery period so it is beneficial to put on sunglasses outside and to attempt and prevent stuffy and warm atmospheres indoors whenever possible. All kinds of contact sports and activities, such as football or martial arts, should be avoided for up to four weeks after surgery, although gentler tasks including swimming can be continued after a fortnight. Also, eye makeup and lotions should be avoided for a week to a month, depending upon the advice given by the ophthalmologist. I find that the vast majority of my patients require a week or two of leave from work after their surgery in order to recuperate absolutely. Some kinds of occupations may request more time away, especially in heavy manual jobs or vocations including lifting. However, it’s highly advisable to use at least some of the time off work to recover and rest, although less strain is put on the eyes themselves and avoidance of matters like rubbing is crucial.
Possible Complications
Now, it is true that, like every other surgical process, transplants carry some risk of complications. However, we should say that transplant surgery is usually very safe. As explained by the experts from the NHS, one of the most important possible complications to be aware of is the risk your body might reject the new organ. Well, we have a brilliant immune system which exists to protect us from illness. In transplant cases, it’s the job of this system to protect our body by attacking and killing off any foreign objects, such as a new organ. This is known as organ rejection. However, all transplant patients are given medication which is specifically designed to help prevent this from happening. In fact, as highlighted, the risk of organ rejection has fallen drastically in the last few decades; in some cases, a patient’s body might not reject their new organ at all. Also, as with any other surgery, it’s also possible to develop an infection following a transplant. Infection is when the body and immune system are overwhelmed by invading microorganisms, such as bacteria. Some of the common signs of infection which patients are told to look out for after transplant surgery include fever, flu-like symptoms, redness or swelling around the operation site, and wound discharge. Again, however, infection risk is managed and minimized through the use of antibiotics and hygiene practice. Plus, all transplant patients are closely monitored after the surgery; this means that any problems, such as infection, are likely to be identified fast. Finally, patients eye transplant cycle development are often told about the dangers of developing PTLD, Post-Transplant Lymphoproliferative Disorder. This is a rare condition which is the result of the white blood cells – the body’s main defense against infection – being overproduced. The disorder can cause the affected lymph nodes and organs to become swollen, giving rise to complications such as breathing difficulties, jaundice and a general feeling of being unwell. However, out of the 300 or so patients who require a kidney transplant each year (and who are therefore most at risk of developing PTLD), only a small proportion will actually suffer from the condition. This is likely to be of some comfort for patients facing an anxious waiting period before or after their surgery. All in all, transplant surgery today can boast high and rising success rates, low rates of complications and ever-shortening waiting lists.

