Myomectomy: Types, Recovery, Risks, and Complications
Myomectomy: Types, Recovery, Risks, and Complications
What is a myomectomy?
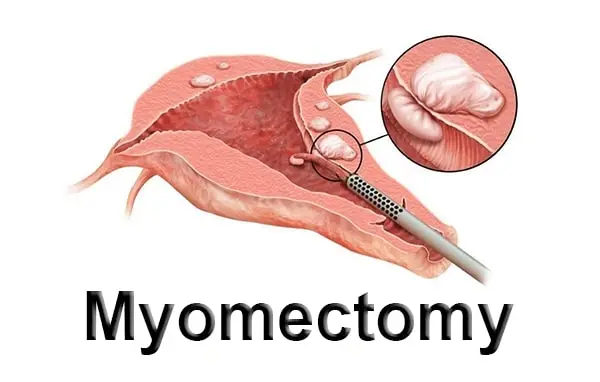
Myomectomy is the term used for the surgical removal of fibroids, which are noncancerous growths, from the wall of the uterus. The traditional method of performing a myomectomy is open surgery, through a large abdominal incision. Often, the fibroids are dissected away from the normal uterine muscle and removed singly through a smaller incision. The type of myomectomy procedure varies depending on the size, number and location of fibroids. Uterine size is also a factor in the choice of myomectomy procedure. Patients typically stay in the hospital for two to five days and require six to eight weeks for a full recovery. Open surgery myomectomy is the most invasive surgical option for fibroid removal. It requires the longest recovery time, but is often the necessary approach for removing very large, deep fibroids. It is well suited for women who wish to maintain fertility because, if the uterine incisions are carefully repaired, the procedure can also be done without compromising the integrity of the uterus for the patient who is interested in childbearing in the future. A laparoscopic myomectomy is a minimally invasive procedure that removes the fibroids without removing the uterus. This procedure uses a power morcellator to divide the fibroids into smaller fragments. These fragments are then removed through small incisions in the abdomen. Due to limitations by the FDA and concern with potential spread of parasitic and uterine malignancies with electric power morcellation, this type of myomectomy is less commonly performed at this time. This approach typically requires less recovery time than open surgery, but morcellation of fibroids may be associated with an increased incidence of fibroid recurrence.
What are fibroids and where do they grow in the uterus?
Fibroids are tumors that grow in the uterus. They are almost always benign (not cancerous). Many women who have fibroids do not have any symptoms. In those that do, symptoms can be influenced by the location, size, and number of fibroids. Fibroids are the most common type of growth found within the uterus. There is no known cause for fibroids; however, it is thought that genetic, hormonal, and environmental factors are all influences. Fibroids can range in number and size from a single growth to multiple growths, and from being very small to very large. Fibroids grow with the womb muscle tissue. The location of a fibroid can influence the symptoms it may cause. Submucosal fibroids grow just underneath the womb lining and can crowd into the uterus cavity. Intramural fibroids grow within the walls of the uterus. Subserosal fibroids grow on the outside of the uterus. Pedunculated fibroids grow on the outside of the uterus and are attached by a narrow stem.
Why is a hysterectomy more common than a myomectomy?
A hysterectomy is the second most common surgery among women in the US and costs 4.3 billion dollars annually, accounting for one-third of all gynecological admissions. The high rate of hysterectomies can be attributed to the fact that this procedure completely cures fibroids and prevents recurrence. Secondly, in cases where women have very large or multiple fibroids, the myomectomy is deemed impractical or excessively risky as it may result in incomplete removal of the fibroids or excessive blood loss. In some cases, surgery is best avoided altogether as the risks may greatly outweigh the benefits. This is particularly true in older women, postmenopausal women, or women in poor health. Women who no longer plan to conceive do not consider fibroid recurrence an issue and opt for a hysterectomy following a surgeon’s recommendation. While myomectomy is the only fibroid treatment that may preserve fertility, it can only be recommended to women with a small number of fibroids located on the inner or outer wall of the uterus. Submucous fibroids and intramural fibroids which distort the uterine cavity can be removed by hysteroscopy or myomectomy, respectively. However, there are few assurances that fibroids will not recur, and the chances of successful pregnancies or pregnancy complications following the procedure are relatively unknown.
When to opt for a myomectomy?
The main reasons to have a myomectomy are:
- Fertility/Pregnancy: If you are infertile and your fibroids are believed to be the cause, a myomectomy can help. Depending on the location of the fibroid, it can hinder your chances of conceiving. Myomectomy has been known to increase fertility levels and the chances of having a successful pregnancy after the procedure has been performed;
- Relief of Symptoms: If you are having pain or if the fibroids are causing other symptoms such as pressure on the bladder or rectum and you have tried medicine or hormonal treatment without relief, myomectomy is a good treatment choice;
If you have been diagnosed with fibroids and are having symptoms such as heavy menstrual bleeding, pain in the pelvic region or pressure on the bladder or rectum, this is a good option. If you are planning to get pregnant, and the fibroid is the likely cause of infertility, a myomectomy is a good option. However, if you are in or past menopause, you may not need to have the fibroid(s) removed, unless they are causing discomfort. If you are not experiencing symptoms, your doctor may monitor your fibroids during routine examinations.
Symptoms of fibroids
Depending on the location of the fibroids, they can cause chronic abdominal pain and/or discomfort. If the fibroid is located low in the uterus, it may obstruct the rectum, causing constipation. If it is located near the spinal column, it may cause back pain. The types and severity of symptoms for fibroids are vast; each woman may have different symptoms.
Effect on pregnancy – location can determine effect. Fibroids located just underneath the lining of the uterus can cause prolonged, heavy periods. Fibroids in the uterine cavity are detrimental to a woman’s fertility. Fibroids located near the lower segment of the uterus can physically obstruct both natural conception and implantation of an embryo. Fibroids anywhere in the uterus can cause pre-term labor. Extrusion of the embryo can occur if the fibroid distorts the shape of the uterine cavity. Women with fibroids have a caesarean section rate of over 30%. This is an invasive surgical procedure with a long recovery time and carries all the risks of major surgery.
Diagnostic tests prior to myomectomy
Laboratory tests
Myoma is always asymptomatic. If we can diagnose symptoms earlier, we can start the treatment earlier. That’s why finding a test to diagnose myoma in the pre-symptomatic or early symptomatic stage is necessary. So we can start the treatment as soon as possible and prevent possible complications. There are two valuable serum tests that have been studied in myoma, which are the measurement of CA-125 and LDH isoenzyme. Measurement of CA-125, a tumor marker used to detect cancers of the ovaries, endometrium, and breast, has provided interesting but inconclusive results. In one study, measurement of CA-125 using a reference laboratory range of normal values (0-35 U/mL) showed that the levels of CA-125 in myoma were no different from the normal population and the correlation of these levels with the size of the myoma was not significant. Suggestions of more significant levels of CA-125 in postmenopausal women with myoma compared with premenopausal women with the same abnormality need to be balanced, as age itself can cause increased CA-125. Because surgery is often performed with endometrial cancer, measurement of CA125 might be useful to determine whether or not there is a malignant tumor associated with the myoma. For the measurement of high CK, high CK reaches significance when accompanied by an increase in lesion size, which is inversely related to the distance with the doctor who intends to operate on a tumor. High CK is also another form of damage to cells and tissues, which correlates with plasmin levels. Today, this indicates the occurrence of myoma tumor in CAM-myoma.
Endovaginal ultrasound
There are two types of ultrasound: transabdominal ultrasounds and transvaginal ultrasounds. For a transabdominal ultrasound, a water-resistant covering is applied to the skin and a scanning probe is moved over a gel to take the images. For a transvaginal ultrasound, a tapered probe is inserted into the vaginal canal and the images can be taken. The latter is proximity imaging in which images can be obtained closer to the target, which allows for a better resolution of the uterus. An ultrasound done for suspected fibroids should be done in close proximity to the time of menses. Fibroids can degenerate, in which there is cystic change and/or bleeding into the fibroid. These degenerative findings can mimic a cancerous process, so it is important to denote the difference if there is suspicion of leiomyosarcoma.
As for diagnosing leiomyomata in women who present with menorrhagia and a known leiomyomata, there are no data that suggest that a pelvic ultrasound will change the management of this patient. If a submucous myoma is suspected, then a hysterosonogram, saline infusion sonohysterogram, and/or hysteroscopy are the tests of choice. Occasionally, a transvaginal ultrasound will suspect leiomyoma, but not be clear on whether it is leiomyoma or leiomyosarcoma. In these cases, mainly if there is thought to possibly be a sarcomatous mass, an MRI will be ordered.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is a valuable tool for diagnosing uterine fibroids, with T1-weighted images revealing them as distinct low signal intensity lesions against the intermediate to high signal intensity of the adjacent myometrium. This clarity aids in distinguishing fibroids from normal uterine tissue. T2-weighted images, on the other hand, depict fibroids as high signal intensity, enabling the visualization of both submucous and intramural fibroids. Utilizing T2-weighted images is crucial for accurately diagnosing submucous fibroids, which might otherwise be mistaken for intra-cavity masses if only T1-weighted images are used. Additionally, three-dimensional MRI imaging provides comprehensive anatomical information, facilitating the assessment of structural abnormalities both before and after surgery by revealing the abnormality’s complete extent and its relationship with surrounding normal structures.
Types of myomectomy
Hysteroscopic myomectomy
When fibroids grow on the inside of the uterine cavity or inside the muscle layer, the size of the uterine cavity can become enlarged giving the impression at an ultrasound examination that a large fibroid exists within it. This can also lead to a diagnosis of unexplained infertility or recurrent miscarriage. This technique is limited to women with submucous fibroids and is not appropriate for those with fibroids deeply embedded in the uterine wall. It is probably more suited to those women who may wish to conceive at a future date, since the impact of surgery on the uterine cavity as well as reducing the risk of uterine rupture in late pregnancy. Hysteroscopic myomectomy is performed using a hysteroscope, a long, thin tube inserted into the vagina in association with a built-in camera to provide a visual guide. No incisions are involved, and the recovery time is swift. As an observer recently mentioned to me, it is « amazing » during the operation to watch the release of the fibroid and seeing the uterus inside just like a map.
Laparoscopically-assisted myomectomy
Laparoscopic myomectomy is a type of myomectomy usually used for removing subserous and intramural fibroids. It is also applicable to the submucus fibroids that have a small connection to the uterus. This procedure can be performed on an outpatient basis, but if the fibroids are numerous and/or large, the patient may require a longer hospital stay. Using general anesthesia, the laparoscope is inserted through the navel allowing the physician to visualize the pelvic region. Three to four additional abdominal incisions are made for insertion of other surgical instruments. A power morcellator can be used to enable removal of even large fibroids through small incisions. The morcellator attaches to the laparoscope and basically shaves off small pieces of the fibroid until it is completely removed from the uterus. This is advantageous because studies show that a myomectomy can weaken the uterus wall and thin down the layer of endometrium. Both of these factors can increase the chances of a miscarriage. Using this tool, fibrous tissue can be removed without taking any uterine tissue and also it stops the growth of new fibroids because the new fibroids are developed from older fibroids. Laparoscopic myomectomy may also reduce post-operative pain and aid in a quicker recovery.
Robotic-assisted laparoscopic myomectomy
Robotic-assisted laparoscopic myomectomy is performed by an experienced surgeon in an operating room. It is considered by many to be the least invasive and most technologically advanced form of myomectomy. The procedure is similar to traditional laparoscopic myomectomy but with a few exceptions. After the uterine cavity is filled with a saline solution to lift the uterus away from other organs, making visualization easier, a small incision is made in or around the navel. This directs the gynecologist to insert a laparoscope to view the internal pelvic cavity and the surgical instruments. If at this point the gynecologist feels that the myomectomy is too complex, the robot can be used as a control mechanism by the gynecologist’s hand to perform the detailed movements of the laparoscopic instruments. This is not often the case, since most laparoscopic techniques are sufficient in the removal of fibroids. Using the laparoscope for visualization, 2 or 3 other small incisions are made in the abdominal wall. Comparing to traditional myomectomy, these incisions are significantly smaller and thus result in decreased amount of recovery time and less scarring. Through these earlier mentioned incisions, the surgeon would either use a particular cutting end called the PK cutlass to perform a myomectomy or use a laparoscopic ultrasound device. This technique can be extensive and thus require more than one setting in the event there are numerous fibroids, and the surgeon would not want to perform the myomectomy on all of them at once to avoid leaving scarring on the uterine wall, which could lead to future complications and even hysterectomy.
Open abdominal myomectomy
An abdominal myomectomy procedure is performed under general anesthesia. The fibroids are removed through an incision made in the lower abdomen. This procedure is recommended for women who have multiple fibroids. Their sizes are what determine if it is possible to have a successful myomectomy. The major drawback of myomectomy is that fibroids may recur. Uterine artery embolization has been successful in shrinking fibroids and reducing the symptoms caused by fibroids. This is a possible alternative to myomectomy.Prior to surgery, an intravenous (IV) line will be started and the area below your navel and up to the « bikini » line will be shaved. A catheter will be inserted into your bladder to keep it empty during surgery. General anesthesia is then administered and you will be asleep during the procedure. An incision is made through your skin and abdominal wall. Once the fibroid is reached, another incision is made in the uterus to remove the fibroid. This is the most popular method to remove fibroids. The uterus is then sutured and the abdominal incision is also sutured.

