Side Effects of Glaucoma Medication
Side Effects of Glaucoma Medication
How common is it for people with glaucoma to experience side effects with their medications?
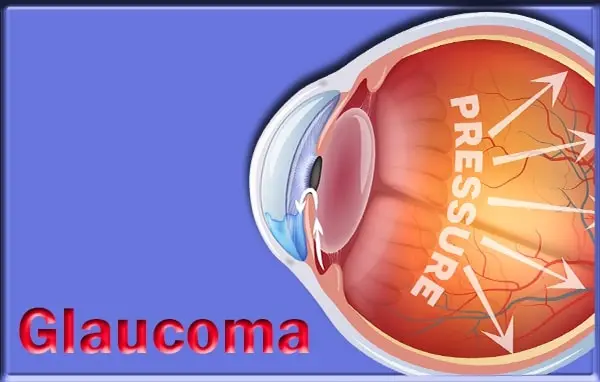
It is estimated that about a third of adults with glaucoma (33%) need to take eye drops every day to keep their eye pressure right to slow down the condition. It is also important to administer the medication as advised by the consultants. Drops prescribed to be used once daily first thing in the morning, or once weekly on the higher side may be associated with significant irritation and redness due to the preservatives present in such drops. Generally, for people with glaucoma, tolerance to the medications differs from an individual to another, where some people are more likely to get side effects by using certain eye drops especially where they are preserved and others are unable to tolerate having eye drops in their eyes, often resulting in lack of compliance. Where patients experience side effects and intolerances that are unacceptable to them, the doctors are often able to offer an alternative treatment or solutions to address the problem. Prof Wong says, « In the twenty-first century, there is a wide array of options in the armamentarium to fight against the progression of glaucoma, including lasers and micro-invasive glaucoma surgery. » Modern glaucoma surgery is now so much more than just making a new drainage pathway for the aqueous humor as we know it historically. He added, « We are able to reduce the pressures and stabilize the vision risk without employing the use of drops with fewer side effects to the patient, using procedures like ‘non-penetrating glaucoma surgery’ where the layers of the eye or the conjunctiva are not broken. »
What sort of side effects do people most commonly experience?
The clear majority of glaucoma eye drops have minimal side effects and, due to modern technological advances, most of these side effects have been eliminated. However, some patients find that they are suffering from discomfort or mild side effects. Most commonly, people experience redness of the eyes, along with stinging and irritation. Additionally, the eyelids may darken or thicken as a result of using glaucoma eye drops. However, all of these side effects are cosmetic in nature and are not dangerous to a patient’s eye health in any way. In extremely rare cases, eye drops can cause more severe side effects. For instance, they can exacerbate existing respiratory conditions such as asthma and cause breathing problems. Other less common side effects which may affect one patient in a hundred include headaches, tiredness, and fainting. On extremely rare occasions, patients have suffered heart palpitations, depression, or liver function problems after using eye drops. However, these possible side effects are listed to make patients aware of the full range of side effects associated with a particular glaucoma eye drop, and they are often detailed on patient information leaflets which accompany the glaucoma medication.
How many days should a person ‘put up’ with side effects before reporting to their eye care specialist?
In answering the question posed in the topic, we should quickly mention that side effects of glaucoma medications generally resolve in 3-4 weeks. However, this should not be misinterpreted to mean that, if side effects last for over 4 weeks, one should wait for the whole period before consulting the doctor. The emphasis here is that, with the discipline of regular drug use as per the doctor’s directions, any abnormal occurring side effect should be reported to the doctor before the end of the period. In essence, unusual and lasting side effects in the eyes should be reported within the first 3-4 days, those affecting the skin around the eyes and forehead region be reported within 6 days and those impacting on the chest and respiratory system within the first 30 days since the person started using a new glaucoma drug. By intelligently outlining these periods, the mystery around which body system is affected by a given side effects is unraveled and the client will quickly know just when to report a given side effect. Ease of use and reduced impediments to timely eye care is often the result when such insights on side effects and treatment are sufficiently explored in glaucoma and eye care instructions.
Why do some preservatives in glaucoma medications cause sore eyes?
The preservatives they use in most eye drops are actually causing inflammation of the surface of the eyes. One example is benzalkonium chloride, which causes oxidative stress on the cells of the cornea. This can make the eyes sore and lead to symptoms like redness, grittiness, and stinging when the drops are put in. Manufacturers are, however, starting to use multi-dose preservative-free systems where preservatives are excluded by protection of the bulk solution from contamination by the outlet flow and surrounding air. These systems help to maintain the sterility of the solution and reduce the risk of contamination by the tip of the bottle touching the eye or face. However, good preservative-free systems do take a lot more of the manufacturer’s resources to ensure the production process upholds the required standards, and it is also a more expensive system to manufacture. Due to budgeting and constraints, and perhaps the greater expense to the NHS, which is ultimately incurred by the increased use of these better treatments, progress is disappointingly slow. In the meantime, it can be helpful to ease symptoms of sore eyes from eye drops by using simple lubricant eye ointments that soothe and coat the surface of the eye. Also, knowing that sore eyes from medication-induced inflammation is only short-lived rather than an irreversible symptom can also provide reassurance while the long, drawn-out process of clinical trials for a newer, preservative-free option.
Where is the tear duct and how long should we press on it after instilling eye drops?
Tears flow from the lacrimal gland, located under the outer portion of the upper eyelid, towards the nasal region. The tear ducts collect tears from the ocular surface and then drain the tears into the nose. Lacrimal puncta are minute openings found above and below in the inner canthus where tears enter the inside of the nose. You can press on the lacrimal sac. This is located between the inner canthus of the eye and the side of the nose. By pressing on the lacrimal sac, you can help to ‘seal’ the drainage pathway so that the tears, which contain the medication, do not drain into the nose and throat. This is particularly important in young children and the unwell who may not understand the need to keep the head tilted after instilling drops. You should press on the lacrimal sac for about one minute after instilling the drops. This will give sufficient time for the drug to be absorbed and to prevent the tears washing it away out of the eyes.
What can a person do to reduce red eyes?
You do not need to bathe your eye in water, but splashing some on your eyes a few times a day to get rid of eyelid swelling and redness can help. Just pat your face dry afterwards to prevent irritation caused by dry skin. Also, you may apply a cold water compress as warm or hot water can cause your arteries to dilate, creating a condition commonly called « blood shot » or « red eyes. » Another home remedy is to give your eyelids a gentle massage to increase the production of tears. By gently running clean fingers over your eyelids and eyelashes, you can help release some of the oils blocking the glands in the eyelids that may reduce tear evaporation. This approach can be useful for fighting off dry eyes. Although remaining hydrated and controlling dry air are important ways to prevent dehydration and evaporation of tears – two causes of red eyes – do not use over-the-counter eye drops to try to moisturize your eyes. These drops may, over time, become addictive in that your eyes will become drier for longer periods of time due to a stoppage in tear production. Instead, try to work in areas with proper air humidity or wear sunglasses or goggles to protect your eyes from irritants, like wind and dust. Using an artificial tear, a lubricating eye drop, can also help to refresh your eyes and alleviate the symptoms of dryness. You should also practice good eyelid hygiene by removing any crusted matter or flaking skin around your eyelids. This is a great way to help control the oil and bacteria around your eyelids which are often contributing to the red eye problem. Work with your eye care specialist to find the most appropriate solution to make sure you maintain a good eye health.
What about itchy eyes that seem to not want to go away?
Dry eye is a common condition in older adults. The eyes do not produce enough tears or the tears dry up too quickly, therefore not keeping the eyes lubricated. However, it is rarely a cause for overly itchy eyes – most of the time dry eye does not cause much itch unless you rub your eyes very hard. Rubbing your eyes excessively can damage the eyes and might cause more harm than good. It can cause micro tears in the cornea – the clear tissue in the front of the eye; it can also worsen dry eye signs and symptoms. Moreover, dry eye might be a sign of a more serious eye condition. Dry eye can be associated with autoimmune disorders and chronic diseases such as lupus, Sjogren’s syndrome, rheumatoid arthritis, and diabetes. When the eye is inflamed and the tears are not normal, it makes the cornea more susceptible to infection. Also, it can damage the front surface of the eye and impair vision. Research has shown that untreated chronic dry eye leads to ocular surface damage, including the development of a specialty of corneal cells due to inflammation and severe dry eye. Such changes to the surface of the eye might cause a person’s contact lenses not to fit or the patient might have decreased tolerance to contact lens wear. Also, those who suffer from chronic dry eye can undergo a loss of their goblet cells – the cells that produce protective tears – on the ocular surface. This loss causes the more clear cells of the cornea to regenerate in a haphazard way and loss of the protective cells can also lead to perpetual irritation of the eye. First, it’s important to get a comprehensive eye examination. An ophthalmologist can help people understand more about the treatment options and provide follow-up care for dry eye. The most commonly used diagnostic tests are examination of the cornea and external areas of the eye using special dyes and high magnification. This approach helps the clinician to visualize and evaluate the integrity of the surface of the eye in a very objective way. Also, the extent of any corneal damage and the healthiness of the cells that produce mucus can be quantified to aid in the diagnosis.