What is corneal transplantation?
What is corneal transplantation?
ABOUT CORNEAL DISEASES
The cornea is the eye’s outermost layer. It is the clear, dome-shaped surface that covers the front of the eye. It is the window of the eye. It is the most important part of the visual system in terms of focusing power. Like the lens of a camera, the cornea helps to focus light on the retina. If the cornea becomes clouded from disease, injury, or hereditary conditions, light is prevented from passing through to the retina, causing a reduction in vision. Cells and tissues of the cornea must be healthy for good vision. Damage or injury to the cornea is a major cause of blindness in the world. Diseases of the cornea are a leading cause of blindness and visual impairment. By far the most common is herpes simplex keratitis, an infection of the cornea caused by the herpes simplex virus. Fungal infections may also cause severe and painful damage. Diseased corneas may become swollen, scarred, or severely misshapen. These conditions can be sight-threatening and may require a corneal transplant to restore lost vision. Earlier the only treatment was to manage with the visual disability. The option of corneal transplantation or grafting has changed a number of lives. Now, people suffering from corneal diseases are aware of the possibility that they can regain good vision. This has minimized the depression that comes with disability.
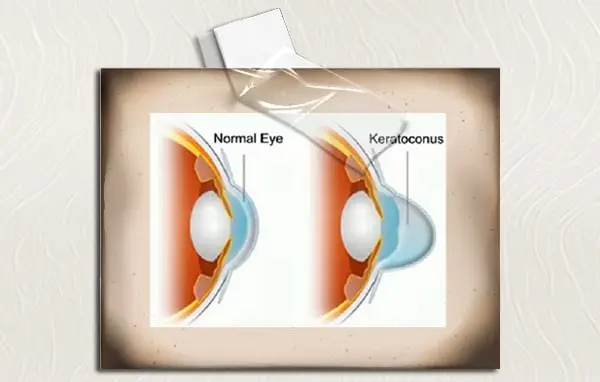
KERATOCONUS
The term keratoconus refers to a disorder characterized by thinning of the cornea. It is commonly bilateral and affects around 1 in 2000 people in the population. The exact etiology is unknown, though some have suggested it is due to collagen abnormalities with the possibility of a genetic predisposition. Environmental factors such as eye rubbing and UV light have also been implicated. The condition usually presents in late teenage years to early 20s, though there is a lot of variation in the age of onset and rate of progression. Initial management is with spectacles though many patients are intolerant due to the high degree of astigmatism. Contact lenses are usually the next step, with many keratoconic patients remaining on contact lenses for many years. Due to the fact contact lenses are so tolerated, corneal transplants are usually a final option when vision is significantly reduced.
KERATOCONUS TREATMENT
When keratoconus is moderate or in its severe state, it cannot be helped by means of conservative treatment. A corneal transplantation may be required. Penetrating keratoplasty (PKP) is the most likely tissue transplant procedure. It is a full-thickness graft which involves removing a button-sized portion of clear cornea from a donor tissue and replacing that of the patient, while discarding the abnormal tissue. Following the surgery, the patient will have to see an ophthalmologist many times over the following year in order to have the eye monitored so that no infections or rejection occur. If the keratoconus is at a very severe stage, a full-thickness graft may not be performed due to the chance of the transplant pushing the progression of the cataract in the eye. In this case, the patient may be referred to have a cataract removed before any corneal work is carried out. An alternative to PKP is Deep Anterior Lamellar Keratoplasty (DALK), which is a more complex procedure where only the anterior portion of the cornea is replaced. Over recent years, a new therapy known as corneal collagen crosslinking has arisen and is now the key to inhibiting the progression of keratoconus. Due to this being a relatively new procedure in comparison to a corneal transplant, many patients may not be familiar with what the therapy involves and what they can expect. Crosslinking aims to halt the progression of keratoconus by saturating the cornea within riboflavin drops and applying controlled UVA light to increase the bonds between corneal fibrils. With these bonds being strengthened, the cornea should stiffen and become more durable in the long term.
It has been suggested that by combining crosslinking with other keratoconus treatments such as intracorneal ring segments and phakic IOLs, the need for a corneal transplant may be reduced. However, a patient should always consult their ophthalmologist to see what treatment is best for their own personal circumstances.
DRY EYES
The very first step in dry eye treatment is a trial of nonpreserved artificial tears 8-12 times a day instilled in both eyes. During the day, hydroxypropyl methylcellulose (Celluvisc) is a good choice for the patient who is using tears more often than six times per day. If tear deficiency is due to a combination of aqueous tear insufficiency and mucin deficiency in the more severe cases of Sjogren’s syndrome, 1% methylcellulose preparations (Tears Naturale Forte) or 1% carboxymethylcellulose preparations (Cellufresh) may be helpful. All of the aforementioned artificial tear products are available over the counter. If the eye is excessively dry during the night, one may add a bland ointment (e.g., Refresh PM) before bedtime to improve ocular comfort. It is to be emphasized that treatment with artificial tears and other ocular lubricants merely palliates the condition by providing symptomatic relief, and a more aggressive treatment regimen is usually required to effect a cure.
If significant aqueous tear deficiency is present, either an alternative to or a supplement for artificial tears is lacrimal punctal occlusion. Punctal occlusion is performed on a trial basis by inserting collagen or silicone plugs into the puncta in the office. If the patient’s symptoms improve over the next 1-2 weeks, punctal occlusion may be accomplished on a more permanent basis with electrocautery or laser cautery of the punctal opening, the latter procedures being performed by an ophthalmologist. Although it is often effective, punctal occlusion is contraindicated in some patients with Sjogren’s syndrome because they may be using punctal medications for associated severe disease of the ocular surface.
OTHER CORNEAL DISEASES
Other corneal diseases encompass a spectrum of conditions that require varying treatments. Mild infections typically respond well to antibiotic drops or ointment. However, more severe infections, characterized by corneal thinning or perforation, necessitate urgent interventions such as gluing, soft bandage contact lens placement, and in critical cases, emergency patch graft surgery. Non-responsive infected corneal scarring may eventually demand corneal transplantation for resolution. Recurrent herpetic eye disease poses another challenge, often leading to painful corneal ulcers and potentially severe immune-mediated corneal disorders. Such cases can be managed through corneal transplantation. Essentially, corneal infection, known as infective keratitis, poses a significant threat to vision. It typically arises when bacteria, fungi, viruses, or parasites invade part of the cornea, usually following ocular surface damage like a corneal abrasion or extended contact lens wear. In rare instances, infections may develop after trauma involving vegetative materials, like plant leaves, which can introduce more virulent fungal or bacterial pathogens.
CONJUNCTIVA
The location of the donor site is determined by the area in need of covering and the type of tissue required. For instance, when treating extensive conjunctival disease involving fornices, cul-de-sacs and lower lid, the entire inferior bulbar conjunctiva may be required as a graft. This may not be suitable if the tissue is to be placed immediately adjacent to the cornea. Instead, it may be preferable to take a tarsal conjunctival graft. Tarsal conjunctiva is less likely to lead to a marked corneal conjunctivalization and may provide a more long-term solution. Tissue harvested from the upper bulbar conjunctiva or limbus is likely to hold corneal epithelium and is unsuitable. The fellow eye is often the best choice for a conjunctival graft. The healthy conjunctiva can be easily assessed and the tissue taken is often of good quality. If both eyes are affected, consideration should be given to any elective surgery that might compromise future vision in the second eye.
Conjunctival transplantation is an integral part of many keratoplasties, particularly when there is limbal stem cell deficiency, as this often involves conjunctivalization of the cornea. Before planning any conjunctival surgery, it is imperative to have a clear idea of the extent and location of the conjunctivalization. This may require meticulous lid eversion and careful examination of the conjunctiva looking for vessels which signal potential for further conjunctivalization. The vessels may need to be marked at the slit lamp with a skin marker for later identification.

