What to know about angioplasty?
What to know about angioplasty?
What is angioplasty?
In modern medicine, angioplasty is recognized as a well-recognized used process to improve heart situation and improve towards a better life. Generally, angioplasty is executed where coronary arteries (which supply oxygenated blood to heart muscle) are blocked due to deposition of fat. Because overtime these gets clogged and the blood flow gets reduced taking the situation it to more severe form called coronary artery disease (CAD) which can further lead to heart attack. Here is where angioplasty is an immediate alternate and lesser risky measure than bypass surgery (certain individuals even opt for it), it’s a treatment to help to restore blood flow to your heart. Reducing damage to the heart muscle and treating CAD will also decrease the risk of heart failure in the future. Angioplasty can be performed at the same time as a PTCA(Percutaneous transluminal coronary angioplasty)./p>
Types
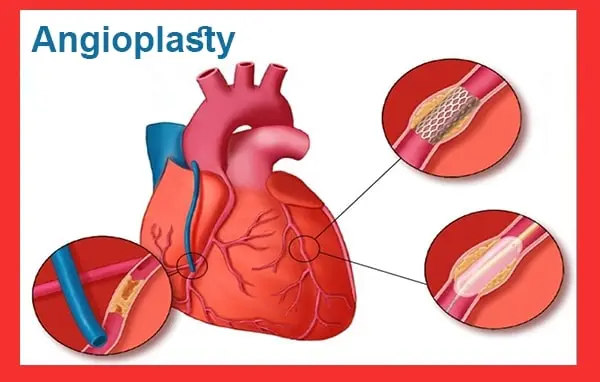
There are two primary types of angioplasty procedures. The most common is balloon angioplasty. In this procedure, a catheter is threaded through the arteries to the site of the blockage. The catheter has a tiny balloon at the end that is inflated once the catheter is in the correct position. Inflation of the balloon is done on site using a guide wire. This flattens the plaque against the wall of the artery, widening the artery lumen and restoring blood flow. After the balloon is inflated, it is deflated and removed from the body. Sometimes angioplasty using a drug-eluting balloon will be used in which medication is released through the balloon in order to better affect the artery. The second type of angioplasty is called stenting. In this procedure, once the balloon has expanded the artery, a wire mesh stent is also expanded and left at the site of the blockage to keep the artery open. Some stents are drug-eluting. This means that they release medication to help keep the artery from narrowing again. Balloon angioplasty does not involve leaving foreign objects within the body and is therefore less invasive than stenting, though stenting has a higher success rate in reducing ischemic events.
How to prepare?
If there is any possibility that you are pregnant or you have allergies to x-ray contrast medium, iodine, or seafood, please inform the nurses and your doctor. On the day of your angiogram. You will then be taken to the Angiography Suite where you will change into a hospital gown and have an IV line inserted. Your doctor will see you before the procedure to explain what will happen and for you to ask any further questions. After the angiogram is complete and it has been determined that you require an angioplasty, your doctor will admit you to the hospital and arrange another date for the procedure to be performed. At this point, your doctor will ask for your informed consent to perform the angioplasty. If you take warfarin or anti-inflammatory drugs such as aspirin or ibuprofen, it is very important that you inform your doctor and the nurse. It may be necessary to stop taking them and start on other medication prior to the procedure. You will be asked not to eat for six hours before the procedure. You can drink water and take your tablets as normal. Bring all your medications with you on the day of the procedure.
Procedure
Access to the blood vessels is gained through a very small incision in the skin, usually at the groin. A plastic tube called a sheath is inserted into a blood vessel, and the flexible catheter is advanced through the sheath into the blood vessels. In some cases, access to the blood vessel is through a needle puncture of an arteriovenous graft or fistula, or through a puncture in a blood vessel in the arm or leg. This approach is used when angioplasty is to be performed on a graft blood vessel. Angioplasty is performed in a specially equipped medical suite or a catheterization laboratory. The patient is usually awake during the procedure, and the degree of sedation is variable depending on the preference of the operator and the patient. Blood pressure and heart rate are monitored during the procedure. The patient is positioned on the procedure table, and the skin is cleansed with an antiseptic solution. A sterile drape is placed around the area. A local anesthetic is injected into the skin.
Risks
The angioplasty procedure results in a low rate of major complications, but it is important for the patient to be informed about them. These risks include death for 1 person in a 1,000. This risk is related to the degree of narrowing of the coronary arteries. Heart attacks occur in about 1-2% of patients undergoing angioplasty. The risk of heart attack is higher when angioplasty does not successfully open an occluded artery, when a large amount of the heart muscle is at risk because of the status of the narrowed artery, and in patients with unstable angina. Damage to an artery. During angioplasty a small amount of damage occurs in the artery (about 15% of lesions undergoing angioplasty are associated with some damage to the artery). This will cause either a small clot to form at the site of injury hence causing a heart attack, or occlusion of the artery at a later date from scarring and constriction of the artery at the site of injury. High lesion complexity is associated with an increased risk of prolonged ischemia and emergency bypass surgery during angioplasty. Other important risks to note are those for certain subsets of patients. Patients who are diabetics have a threefold increase in mortality from coronary events occurring during or after angioplasty. This is because atherosclerosis in diabetics is more diffuse and leads to a higher possibility of occlusion of the arterial lumen from the debris becoming dislodged during angioplasty. Severely symptomatic patients (ie. patients with class IV angina) have a higher risk of myocardial infarction during angioplasty and more serious complications in the course of those MI’s.
Recovery
It is common to have a sore and slightly numb groin for a day or two. You may also develop a benign hematoma (collection of blood) that causes bruising at the site. Apply a cold pack (crushed ice in plastic bag) to the area for 15 minutes each hour and take it easy for the first couple of days after the procedure. You can resume all your usual activities including bath or shower on the third day after having seemed improvement in the soreness at the biopsy site. Avoid heavy lifting or vigorous exercise for a week after the procedure. This will reduce the chance of re-bleeding into the artery. On the seventh day after the procedure, you can usually restart aspirin or other anti-platelet medication if it was stopped for the angioplasty. When you first wake up, the nurse will probably remove the introducer sheath from the artery in your groin. To do this, pressure is applied to the biopsy site for 20 to 30 minutes. The nurse then puts a clamp on the artery, and you need to keep your leg straight for another four to six hours to avoid bleeding from the biopsy site. This is the only time you have restricted activity. You must remain lying in bed for the first hour and a half after the clamp is removed. You may get up to use the bathroom, but spend the majority of the time sitting or lying down. Do not walk or stand for long periods for the rest of the day. This will minimize the likelihood of bruising or bleeding at the site of catheter insertion. After your angioplasty, if it was uncomplicated, you can expect to stay in the hospital for 12 to 24 hours. You should be able to return to work within a week.

