What You Need to Know About Prostate Surgery (Prostatectomy)?
What You Need to Know About Prostate Surgery (Prostatectomy)?
What is prostate surgery for?
Open radical prostatectomy (ORP)
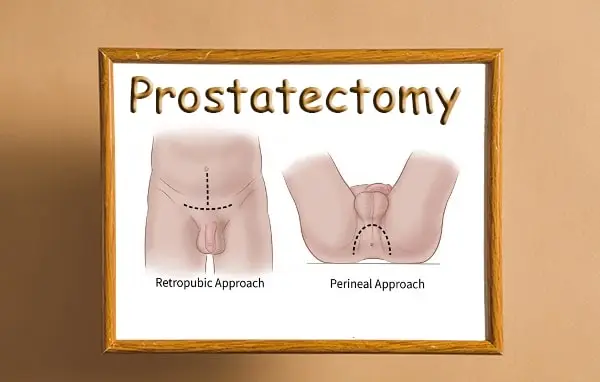
There are various types of ORP that can be used, however, each different to fit the preference and skill of the surgeon. The three most commonly used procedures are the perineal, retropubic, and suprapubic surgery. The perineal surgery uses an incision made in the perineum, the area between the anus and the scrotum. This method allows the surgeon to remove the lymph nodes around the prostate while checking for cancer spread on other surrounding areas. The retropubic surgical method makes an incision in the lower abdomen to access the prostate. The suprapubic surgery also makes an incision in the abdomen and is similar to the retropubic method; however, it allows the surgeon access to lymph nodes in different areas of the pelvis. Each of these procedures have their advantages and disadvantages and should be discussed with the doctor.The open radical prostatectomy is one of the common treatments for prostate cancer. This is the method used in 60-2% of the time. It is not used often in men who are in the early stage of this disease. The low risk and early stage cells tend to have a high 10-year disease-free survival rate in most men. The ORP is most used in the men who may have the faster developing cells or may have cancer that has spread to parts of the tissue surrounding his prostate.
Radical retropubic prostatectomy
Radical retropubic prostatectomy is done with the patient in the low dorsolithotomy position and the abdomen is opened with a 15cm lower abdominal incision. In this procedure, dissection of the prostate is done through an incision made in the space between the rectum and the back of the pubic bone. The seminal vesicles and ampulla of the vas deferens are separated from the bladder and the prostate is freed by cutting the bladder neck. Measures to improve disease control may involve deeper removal of adjacent tissues thought to be at risk of involvement in order to widen the tumor-free margin. This may include wider excision of the neurovascular bundles thought to be responsible for control of erection. An attempt to confirm the extent of disease to allow proper patient selection will be undertaken with TRUS and biopsy findings. The detailed anatomy of the retro pubic space has allowed recent development of a minimally invasive laparoscopic technique. This technique has the advantage of reducing blood loss and hastening recovery but outcomes in terms of long-term disease control and quality of life remain to be seen.
Radical perineal prostatectomy
During this procedure, the surgeon will make an incision in front of the anus and behind the scrotum. In this way, the perineal approach avoids cutting through the muscle of the abdominal wall and may be a good option for men who have had lower abdominal surgery or have other conditions that would make the retropubic approach more difficult. The wound leaves a scar, but this is usually in a place where it is not noticeable. The surgeon then separates the penis and scrotum from the pubic bone, and this tissue is set aside. This allows the surgeon to easily and directly access the space between the pelvis and the prostate gland, where the major blood vessels to the prostate are located, and this may help reduce blood loss during the surgery.At this point in the surgery, the patient is usually given a blood thinner to prevent blood from clotting in the pelvic area after the surgery. This is because the swollen tissue and the lack of movement that occurs during recovery from prostate surgery put the patient at an increased risk of blood clotting. With the prostate now removed, urine will flow differently within the body, and a new passage is made to connect the urethra with the penis. This is done by removing the old section of the urethra that passed through the prostate and making a new opening in the urethra that lines up with the bladder. This is typically accomplished by placing a catheter in the patient’s urethra, which will remain in place for 1-2 weeks after the surgery.The tissue surrounding the prostate, known as the seminal vesicles, is also removed during surgery, and this will change sexual function as semen no longer contains sperm. This is often the most difficult part of prostate removal surgery due to the proximity of the vesicles to the nerves that control erection, ejaculation, and orgasm.
Laparoscopic prostatectomy
Laparoscopic radical prostatectomy (LRP)
Laparoscopic radical prostatectomy (LRP) is a minimally invasive approach to remove the prostate. Unlike open radical retropubic prostatectomy (RRP), which requires an 8-10 inch incision, LRP requires only 5 small (1/2 inch) incisions. The surgeon uses one incision to insert a camera, which provides a magnified view of the surgical area, and the other incisions are used to manipulate the instruments to perform the surgery. In addition to being less invasive, LRP may also result in less blood loss, a shorter hospital stay, and a quicker recovery compared to RRP. After removal, the prostate is placed in a bag and removed through one of the small incisions. This is in contrast to RRP, in which the prostate is removed through an incision above the pubic bone. Bagging the prostate decreases the risk of cells seeding into surrounding structures. This is called port site metastasis, and though it is rare, it has been seen in some patients who undergo RRP. Also, the intraoperative use of frozen section to determine if the cancer is confined to the prostate is more difficult to perform in an LRP compared to an RRP. This is because the frozen section analysis is done by shaving thin layers of the prostate and examining each layer under a microscope. The freezing process causes the prostate tissue to harden, and it is difficult to shave thin layers off the prostate when it is so firm. However, the frozen section is performed in a similar manner to RRP once the LRP surgeon gains enough experience, as many surgeons work out techniques to shave thin layers off the prostate during LRP. A similar limitation to LRP compared to RRP is that the nerve sparing procedure is more difficult to perform in an LRP. This is because the nerve bundles are more difficult to visualize in LRP, and it is harder to distinguish between the cancerous and normal prostate tissue. However, the ability to spare the nerve bundles is an important factor in postoperative potency and continence outcomes, and many patients who undergo LRP are hopeful that the nerve sparing procedure can be effectively performed. Ultimately, while there are downsides and increased difficulty in performing certain procedures associated with LRP compared to RRP, LRP provides a surgical treatment option for prostate cancer with the advantages of being less invasive, having less blood loss, a shorter hospital stay, and a quicker recovery.
Robotic-assisted laparoscopic radical prostatectomy (RALRP)
This is the most technically advanced form of minimally invasive surgery. RALRP is performed under general anesthesia and involves making six small incisions instead of one long incision. A thin tube containing a light and lens (laparoscope) is guided through one of the incisions, magnifying the surgical site onto a video screen. The surgeon is seated at a console viewing the 3-D images and manipulating handles that control the instruments. The instruments translate the surgeon’s hand movements into precise micro-movements. The surgeon’s ability to view the surgical site in 3-D and the increased dexterity to spare delicate nerves and surrounding tissue contributes to the preservation of continence and potency. RALRP procedures are complex and the learning curve for the surgeon is steep. Patients should seek surgeons who have performed a large number of procedures and who are experienced with open radical prostatectomy. Outcomes at one year are similar between patients who undergo RALRP and open radical prostatectomy. However, long-term data is not yet available and many experts caution patients about the perception of high risk associated with performing radical prostatectomy where the cancer is often localized and curable with observation.
Are there differences between ORP, LRP, and RALRP?
There are pros and cons to each of these surgical approaches that relate to the surgeon’s experience and skill, as well as to patient factors such as body habitus, prior surgery, and prostate size. Although the data is early for the RALRP, improvements in potency and continence have been suggested by some investigators. The RALRP benefits from low blood loss and postoperative pain, a short hospital stay, excellent visualization of anatomic structures, and the potential for earlier return of urinary continence and erectile function. Also, men with large prostates or a history of prior surgery may not be well suited for ORP due to a higher risk of adverse events, such as blood loss and prolonged catheterization. This may not be the case for LRP, as large prostate size is a relative contraindication for this approach. Lastly, older men and those with significant medical comorbidities may choose RALRP or a nonoperative strategy due to similar cancer control and lower risks of adverse events. These potential benefits should be weighed against the higher cost of the robotic approach and the possibility that the long-term outcomes of RALRP may not justify the initial expense.
Types of prostate surgery that help with urine flow
Prostate laser surgery
GreenLight laser surgery, also known as photoselective vaporization of the prostate, is a recent advance in the treatment of benign prostatic hyperplasia (BPH). During GreenLight laser surgery, a thin fiber is inserted through the penis into the urethra; no incisions are required. Pulses of light are delivered through the fiber, and the energy emitted by the light is absorbed by the blood. Focal point coagulation necrosis of BPH tissue occurs and ultimately the tissue vaporizes, and 2-3 grams are removed during each procedure. This is a relatively bloodless surgery and patients are able to go home with a catheter for overnight only. This is same day surgery, the catheter is removed in the morning and patients are able to urinate and go home without having a catheter. This is a well-tolerated procedure with an 80-85% success rate at 5 years. This procedure is done in proper candidates who are not on blood thinners and have no active infections. This procedure cannot be done in men who are on blood thinners due to the high risk of severe bleeding and it is not indicated in patients who have bladder diverticulum, bladder stones, or have a neurogenic bladder. This procedure is sometimes used to treat acute urinary retention. This is an option for those patients who do not wish to discontinue or interrupt their anticoagulation regimen.
Endoscopic surgery
An alternative to the TURP is to gain access to the inside of the prostate through an endoscope, a metal sheath containing a fiber-optic light source and a tiny camera, which sends a magnified image to a video screen. Using the endoscope, the surgeon can see the position of the surgical instruments and the tissue that is being removed. There are three different techniques for endoscopic surgery, the most common being known as TURiP (transurethral resection in the prostate). This involves cutting away at the enlarged prostate tissue which is blocking the urethra using a specially designed telescope which can reach the innermost parts of the prostate gland. This is thought to be less damaging to the surrounding areas than the standard TURP, but has been shown to have similar effectiveness in terms of reducing symptoms initially.The other two techniques, known as laser surgery, involve using different types of laser to burn away the excess tissue blocking the urethra. The advantage of this type of procedure is that it can be done under local anesthetic and is sometimes performed as a day case, with patients returning home the same day. Laser surgery has not been performed for as long as TURP and TURiP and may not be as effective in the long term, but early results suggest that it does have a good success rate and may be an option for some patients.
Side effects of prostate surgery
Urinary problems
The most common form of urinary incontinence following prostatectomy is stress incontinence, occurring in approximately 10-20% of patients. This type of incontinence arises due to the effects of taking the prostate and the damage to the sphincter muscle during surgery. Leakage may be a small amount, for example when you cough or sneeze, or in more severe cases, leakage can occur with any activity. 1-2 pads per day are usually sufficient to control leakage. If urinary continence does not improve over time, where possible, underlying causes such as prostate re-growth or damage to the bladder outlet should be assessed. Measures for stress incontinence include exercises to strengthen the pelvic floor muscles, medications, or surgical intervention. An artificial urinary sphincter may be implanted to help return control of urination. Patients may experience urinary incontinence that can last several weeks to many months. It may take up to a year to regain full bladder control. The type of incontinence experienced depends on the type of surgery undertaken. Urge incontinence is a feeling of needing to pass urine and leaking before reaching the toilet. Stress incontinence is leaking of urine with activities such as walking, lifting, and coughing.
Erectile dysfunction (ED)
Prostate surgery is one of the main causes for developing erectile dysfunction. The chance of developing erectile dysfunction depends on the age, the disease which has prompted treatment, the type of treatment, and the surgeon’s skill. The damage is more common with the radical prostatectomy procedure, and the patient’s age at the procedure affects the risk of erectile dysfunction developing. More than 50% of patients under 60 years old will have some trouble with erectile dysfunction after the surgery. The use of Viagra may be helpful in achieving erections and comes highly recommended to promote healing of the nerves, although its reliability is still in question. There are several different ways to treat erectile dysfunction. The simplest way to treat it is by doing nothing at all, as there is a chance that the sexual function may return on its own. If this is not effective, medication or devices to increase blood flow to the penis and/or hormone replacement therapy may be used. The most common and effective treatment is called intracavernous injection, whereby a small needle is used to inject medicine into the side of the penis. This will have to be taught to the patient by the doctor, and up to 85% of men can achieve erections with this therapy. If all else fails, a penile prosthesis may be inserted via a surgical procedure.
Sexual dysfunction
Why is it that surgery affects your erectile function? The nerves that stimulate erection are located on the side of the prostate gland and are extremely delicate. When a surgeon operates to remove the prostate gland, there is a risk that these nerves can be damaged or removed, in order to try and remove all of the cancer cells. If the cancer is localized and the nerves are not damaged this means that you have a higher chance of keeping your current level of erectile function post-operatively. This would be determined by an erection assessment with an anesthetist before your surgery. The assessment would test if you are able to achieve and maintain an erection with the use of an injection into the base of the penis, to cause an erection by dilating vessels and triggering the same mechanisms involved in the physiological process. This assessment can only indicate the potential for keeping erectile function and is a good predictor for some men. Sexual dysfunction following prostate surgery is one of the most common, yet least talked about side effects. What most people are not aware of is that the rates of erectile dysfunction after a radical prostatectomy is somewhere between 40-70%. The wide variety in this range is because erectile function studies are poorly conducted, with a response rate on questionnaires often being less than 50%. Often people who are not experiencing a problem are less likely to fill it in a questionnaire on their sexual function. The true percentage of men who have erectile dysfunction after prostate cancer treatment is probably much higher than 70%. Other forms of prostate surgery such as TURP or Brachytherapy can also affect your erectile function, but not in so many cases.

